Liver Disease Progression
There is no accurate way to predict the course of chronic hepatitis C in an individual person.
Introduction
Throughout this site, you will often read that chronic hepatitis C and its treatments affect each person differently. The broad range of variability observed between persons living with hepatitis C is especially true of disease progression. There is no accurate way to predict the course of chronic hepatitis C in an individual person.
This section provides information about possibilities that might happen. Remember, none of the situations discussed in this section will necessarily happen to you. However, it is important to be aware of the possibilities so that if any of them do occur, you will be prepared and better able to make good decisions.
About the Liver
The liver is the largest internal organ of the body. In a normal adult, the liver weighs 3½ to 4 pounds (1,300 to 1,500 grams). It accounts for about 2.5% of the total weight of the body. The liver is wedge-shaped (see Figure 1). It measures approximately 7 inches (14 cm) across by 5½ inches (18 cm) along its diagonal.
The liver is divided into two main lobes, the right and the left. The right lobe is slightly larger than the left and extends down the right side of the rib cage. The left lobe extends from the right lobe to about the middle of the abdomen. There are also two minor lobes of the liver, the caudate and quadrate lobes. Fibrous ligaments separate the lobes. All lobes of the liver perform the same functions. The entire liver is enclosed in a fibrous sheath called Glisson’s capsule.
Figure 1. Anatomy of the Liver
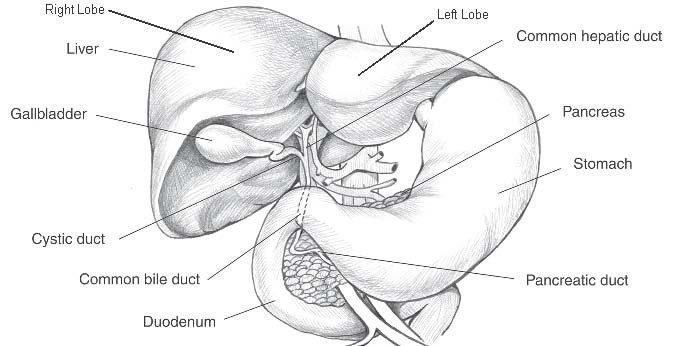 *Courtesy of National Institute of Diabetes and Digestive and Kidney Diseases
*Courtesy of National Institute of Diabetes and Digestive and Kidney Diseases
 The liver is located on the right side of the abdominal cavity just below the lungs and diaphragm, the muscle that separates the chest cavity from the abdominal cavity. The liver is packed so tightly into the abdomen that the right kidney, parts of the large and small intestines, and the stomach actually leave impressions on its surface. Even the ribs and muscle bands of the diaphragm make indentations on the surface of the liver.
The liver is located on the right side of the abdominal cavity just below the lungs and diaphragm, the muscle that separates the chest cavity from the abdominal cavity. The liver is packed so tightly into the abdomen that the right kidney, parts of the large and small intestines, and the stomach actually leave impressions on its surface. Even the ribs and muscle bands of the diaphragm make indentations on the surface of the liver.
Approximately 25% to 30% of the blood coming from the heart goes to the liver. Although there are no lymph nodes in the liver itself, it produces over ⅓ of the body’s lymphatic fluid. The fluid drains into lymph channels and lymph nodes in the abdomen.
The hepatitis C virus (HCV) enters the body through the blood stream. It is carried by the blood to the liver where it infects hepatocytes (liver cells). HCV reproduces in liver cells. Studies suggest HCV is also reproduced in cells of the blood and bone marrow.
Once diagnosed with hepatitis C, you will have many tests to determine the status of your disease. For detailed information on the tests you may have and why, see Laboratory Tests and Procedures.
Checking blood levels of the liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST) is one way to tell if liver cells are dying. When liver cells die, ALT and AST are released into the blood. After an abnormal amount of liver cell death, ALT and AST levels rise over a period of 7 to12 days and then slowly return to normal. If liver cells continue to die in abnormally high numbers over time, ALT and AST levels remain elevated.
ALT and AST levels provide information about liver damage, but do not provide information about how much liver repair is taking place. Studies show that liver enzyme levels do not predict disease outcome. You can have normal liver enzyme levels and still have liver damage.
Liver enzymes also provide no information about how well the liver is functioning.1,2 Your liver can maintain its many functions despite a remarkable amount of damage. Therefore, it is important to look at the results of other test such as albumin, bilirubin, prothrombin time, and platelet count to determine how well your liver is functioning.
Liver enzymes such as AST and ALT reflect liver damage but not liver function.
Liver enzymes do not predict disease outcome.
Stages of Disease Progression
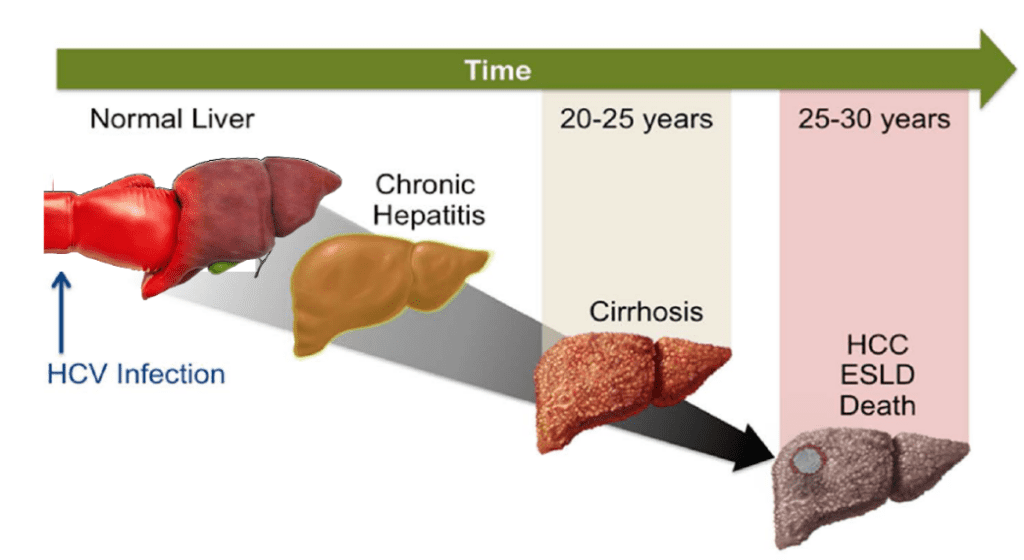
Like other liver diseases, HCV disease progresses in stages. The usual progression is from inflammation to fibrosis to cirrhosis . Cirrhosis can progress to end-stage liver disease and/or can give rise to liver cancer.
Inflammation
Inflammation is the body’s normal response to injury or infection. When the liver is inflamed, there is an overabundance of special cells called inflammatory cells in the liver. Inflammation is labeled chronic when it persists for prolonged period of time.
Chronic inflammation can lead to changes in liver structure, slowed blood circulation, and the death of liver cells (necrosis). Prolonged liver inflammation can eventually cause scarring, which is called fibrosis. By controlling liver inflammation, you can potentially control progression to fibrosis.
Fibrosis
Fibrosis is the harmful outcome of chronic inflammation. Fibrosis is scar tissue that forms as a result of chronic inflammation and/or extensive liver cell death. Your healthcare provider uses the amount of fibrosis in your liver as one way of evaluating how quickly your hepatitis C appears to be progressing. Knowledge of approximately when you were initially infected with HCV is a great help in determining your rate of disease progression.
 Cirrhosis
Cirrhosis
When fibrosis becomes widespread and progresses to the point that the internal structure of the liver is abnormal, fibrosis has progressed to cirrhosis. Cirrhosis is the result of long-term liver damage caused by chronic inflammation and liver cell death. The most common causes of cirrhosis include viral hepatitis, excessive intake of alcohol, inherited diseases, and hemochromatosis (abnormal handling of iron by the body).
Cirrhosis leads to a reduction in blood supply to the liver. The loss of healthy liver tissue and reduced blood supply can lead to abnormalities in liver function. Even when liver disease has progressed to cirrhosis, it may still be possible for the damage to be at least partially reversed if the underlying cause can be eliminated. Cirrhosis progression can usually be slowed or even stopped with effective treatment.
People are often surprised to learn that you can have cirrhosis of the liver and not know it. The onset of cirrhosis is usually silent with few specific symptoms to signal this development in the liver.
As scarring (fibrosis) and liver cell destruction continue, some of the following signs and symptoms may occur:
- loss of appetite
- nausea and/or vomiting
- weight loss
- change in liver size
- gallstones
- generalized, persistent itching ( pruritus)
- jaundice
Despite the seriousness of cirrhosis, large numbers of people live many, many years with cirrhosis without symptoms and without progressing to liver failure.
Once cirrhosis develops, it is very important to avoid further progression of the disease. Consumption of alcohol in any form, including such things as certain mouthwashes and cough medicines, must be completely avoided by people with cirrhosis. If you have cirrhosis, this may be a time to reevaluate your treatment goals. If you have not been cured, you may want to consider it. It may also be time to look into other means of improving your liver health.
Liver Cancer
Most people with HCV never develop liver cancer. Nonetheless, people with HCV are at an increased risk for liver cancer. The presence of cirrhosis and/or having been infected with HCV for more than 20 years further increases the level of risk. The development of liver cancer (hepatocellular carcinoma) is most commonly seen in people who have cirrhosis,3 but rare cases of this cancer have been reported in HCV patients without cirrhosis.4 The reported risk for the development of liver cancer among HCV-positive patients with cirrhosis is 1% to 2% per year.5
Liver cancer screening remains controversial in the United State because there are no large scale clinical trials to prove that such testing improves overall liver cancer survival rates. However, liver cancer screening among people with chronic hepatitis C is widely accepted and practiced by most hepatologists and gastroenterologists.
Liver cancer is life threatening, so do not delay telling your healthcare provider about any changes in your symptoms. If you have cirrhosis, you need to be followed closely by a healthcare provider who will monitor you with the appropriate liver cancer screening tests such as liver ultrasonography and/or alfa-fetoprotein levels.
Assessing Liver Fibrosis
-
There are a few ways to assess liver fibrosis ranging from invasive to noninvasive approaches. See the table below for more information on the range of options available to patients to assess liver fibrosis.
Test Pro Con Liver Biopsy – this is a medical procedure where a small portion of the patient’s liver is extracted inside of a needle and analyzed under a microscope. – May be helpful in diagnosing other potential liver conditions
– There is a validated scoring system
– invasive and painful for the patient
– high sampling error
– expensive
Fibroscan – a specialized ultrasound machine that measures liver scarring. – noninvasive and painless
– easy to repeat testing over time
– Food intake prior to scan may skew results
– May be hard to differentiate between the nuanced levels of fibrosis
Direct Serologic Markers
i.e. lab-based tests that are specialized labs designed to measure specific liver function, fibrosis and inflammation
– Minimal discomfort for patient
– can be easily re-evaluated over time
-May be hard to differentiate between the nuanced levels of fibrosis Indirect Serologic Markers
Indirect serologic markers are calculator-based tools that use a patient’s existing labs (AST, platelet) to determine a potential level of fibrosis.
Links to Clinical Calculators
– helpful when combined with other information (clinical findings, history, etc.)
– easily accessible online calculators using labs typically found in a patient’s chart
-indirect and uses other markers to give an indication
– may be hard to differentiate between the nuanced levels of fibrosis
Other Liver Diseases
Fatty Liver (Steatosis Or Steatohepatitis)
Fatty liver is a general term indicating the accumulation of fat in liver cells. Steatosis is the presence of fat in liver cells without inflammation. Steatohepatitis is the presence of fat in liver cells with inflammation. You may hear other terms to describe fatty liver, depending on your medical condition.
NAFL – nonalcoholic fatty liver
NAFLD – nonalcoholic fatty liver disease
NASH – nonalcoholic steatohepatitis
Fatty liver is emerging as a major medical problem. Obesity affects up to 35%6 of adults in the U.S. population and 17% to 33% have NAFLD.7 Approximately one-third of people with NAFLD will have progressive liver disease.8
For the hepatitis C patient, fatty liver is another factor that may accelerate in the progression of fibrosis.9 A liver biopsy can determine both the presence of fat in the liver and the level of fibrosis. This information will allow your healthcare provider to counsel you about your risk of progressive liver disease.
Alcohol consumption can increase the amount of fat in the liver and is the most common cause of fatty liver. The association between fatty liver and alcohol is another very important reason for you to refrain from drinking any alcohol. However, not all cases of fatty liver are caused by alcohol use. Diabetes and high triglycerides are also associated with fatty liver and should be managed closely by your healthcare provider.
The liver must metabolize any fat that is not eliminated through the intestinal tract. If you eat excessive amounts of fat, the amount that goes to your liver may be too much for it to metabolize. Excess fat that is not metabolized begins to accumulate in the liver. This accumulation of fat can cause inflammation. Inflammation can lead to scarring, which may eventually lead to decreased liver function. Therefore, it is important not to have excessive amounts of fat in your diet. It is particularly important to limit your intake of animal fat because animal fat is especially difficult for the liver to metabolize.
Achieving or maintaining your ideal body weight (a body mass index [BMI] of approximately 20 to 25) and limiting the amount of fat in your diet are important for your liver health. Your BMI is calculated by taking your weight (in kilograms) and dividing by your height (in meters) squared. Normal body weight not only helps your liver but can also improve your energy level, reduce hypertension, and lower your risk of heart disease. Regular exercise can help you maintain a normal body weight and avoid the development of fatty liver.
People with fatty liver often have high blood sugar and lipids such as cholesterol and triglycerides. If you have a fatty liver, your healthcare provider should monitor you for the development of these problems.
Some medications and other substances can cause fatty liver. Be sure to review all of your medications with your healthcare provider and avoid the following, if possible.
- alcohol
- amiodarone (anti-arrhythmia medicine)
- methotrexate (arthritis medicine)
- high doses of vitamin A
- tetracycline (antibiotic)
- cortisone (steroid medicine)
- prednisone (steroid medicine)
Systemic Complications of Hepatitis C
Although the effects of HCV on the liver are most visible, the virus can affect other body systems and organs. This results in extrahepatic (outside the liver) conditions or manifestations of chronic hepatitis C.
Many autoimmune diseases occur as secondary diagnoses after a primary diagnosis of chronic hepatitis C or in association with hepatitis C. Some examples of these diseases include:
- type 2 diabetes
- mixed cryoglobulinemia
- thyroiditis
- erythema nodosum
- erythema multiforme
- glomerulonephritis
- hypothyroidism
- lichen planus
- polyarteritis
- urticaria
- porphyria cutanea tarda
- polymyalgia
- B cell lymphoma
- Mooren corneal ulcers
There is much controversy regarding the true cause of the many so-called HCV-related conditions that have been reported. Some of them probably are related to hepatitis C. Others probably are not, and occurred by chance in a few individuals unrelated to HCV. Many studies on this topic come from clinics that treat only specific diseases, which may skew the study findings.
The way HCV produces extrahepatic conditions and the true prevalence of these conditions is the subject of ongoing research. The link to type 2 diabetes has been studied by numerous groups and it appears that HCV causes insulin resistance.10-13 In other HCV-related extrahepatic conditions, HCV stimulates the immune system to produce autoimmune antibodies, antibodies against the body’s own tissues. This appears to be the mechanism for HCV-related thyroid and blood disorders.
We are hopeful that ongoing research will help clarify both the mechanism of these potentially debilitating conditions and new treatments to help alleviate the suffering caused by them.
Summary
The question of whether it is the virus or the person infected by the virus that determines how HCV disease will progress is an active area of medical research. At this point, several personal factors and several viral factors have been identified that may influence the rate of HCV disease progression.
Personal factors related to disease progression include some variables you can control. The consumption of alcohol can markedly affect disease progression. The amount of fat in one’s diet, and body weight can also influence disease progression and treatment outcomes. Your environment, diet, exercise plan, lifestyle, and support system may all be important factors that could affect the course of your HCV infection.
Progression of chronic hepatitis C in any given person cannot be predicted. The majority of people will not progress to cirrhosis. However, the seriousness of this disease for people with advanced cirrhosis is beyond question. If you follow the progression of your disease with all the tests available to you, you will be in a better position to make informed decisions about your treatment options.
We are confident that ongoing research will improve the ability to predict disease progression and intervene more effectively.
References
Information in this section has been updated and adapted from Hepatitis C Choices 4th Edition, Liver Disease Progression written by Lorren Sandt
- Datz C, Cramp M, Haas T, Dietze O Nitschko H. The natural course of hepatitis C virus infection 18 years after an epidemic outbreak of non-A, non-B hepatitis in a plasmapheresis centre. Gut. 1999;44(4):563-567.
- Persico M, Persico E, Suozzo R, et al. Natural history of hepatitis C virus carriers with persistently normal aminotransferase levels. Gastroenterology. 2000;118(4):760-764.
- El-Serag HB. Epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2001;5:87-107.
- De Mitri MS, Poussin K, Baccarini P, et al. HCV-associated liver cancer without cirrhosis. Lancet. 1995;345:413-415.
- Fattovich G, Giustina G, Degos F, et al. Effectiveness of interferon alfa on incidence of hepatocellular carcinoma and decompensation in cirrhosis type C. J Hepatol. 1997;27:201–205.
- Ogden CL, Carroll MD, McDowell MA, Flegal KM. Obesity among adults in the United States – no change since 2003—2004. NCHS data brief no 1. Hyattsville, MD: National Center for Health Statistics, 2007.
- Farrell GC, Larter CZ. Nonalcoholic fatty liver disease: from steatosis to cirrhosis. Hepatology. 2006 Feb;43(2 Suppl 1):S99-S112.
- Duvnjak M, et al. Pathogenesis and management issues for non-alcoholic fatty liver disease. World J Gastroenterol. 2007 Sep 14;13(34):4539-50.
- Castera L, Hezode C, Roudot-Thoraval F, et al. Worsening of steatosis is an independent factor of fibrosis progression in untreated patients with chronic hepatitis C and paired liver biopsies. Gut. 2003;52:288-292.
- Delgado-Borrego A, Liu YS, Jordan SH, et al. Prospective study of liver transplant recipients with HCV infection: evidence for a causal relationship between HCV and insulin resistance. Liver Transpl. 2008 Feb;14(2):193-201.
- Albert L, et al, High Prevalence of Glucose Abnormalities in Patients With Hepatitis C Virus Infection. Diabetes Care Volume 27, Number 5, May 2004
- Hui JM, Sud A, Farrell GC, et al. Insulin resistance is associated with chronic hepatitis C virus infection and fibrosis progression [corrected]. Gastroenterology. 2004 Feb;126(2):634.
- Shintani Y, Fujie H, Miyoshi H, et al. Hepatitis C virus infection and diabetes: direct involvement of the virus in the development of insulin resistance. Gastroenterology. 2004 Mar;126(3):840-8
