Alcohol and Hepatitis C
Eliminating alcohol is the single most important lifestyle change you can make to decrease your risk for developing complications from chronic hepatitis C.
The three most important factors associated with rapid progression of chronic hepatitis C are age over 40 years, male gender, and alcohol consumption.1-3 You cannot change your age or gender, but you can eliminate alcohol.
Eliminating alcohol is the single most important lifestyle change you can make to decrease your risk for developing complications from chronic hepatitis C.
“But I Only Drink Beer”
Most people in the United States who drink alcohol do so socially. You may be used to having a glass of wine with dinner or a mixed drink at a party. However, if you have hepatitis C, any consumption of alcohol is potentially damaging to your liver. Whether alcohol is consumed in a drink, cough syrup, or another nonprescription product, alcohol is an enemy to people infected with the hepatitis C virus (HCV). Alcohol should be completely avoided.
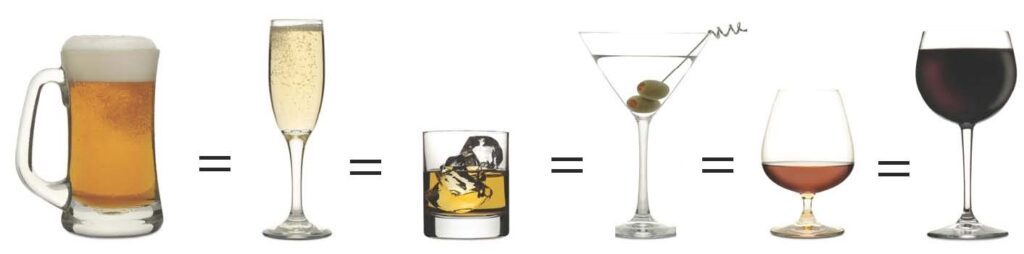
The primary cause of liver damage from alcohol is the alcohol itself. It makes no difference whether the alcohol is contained in beer, wine, or hard liquor. A twelve–ounce can of beer contains the same amount of alcohol as a four-ounce glass of wine or a one-ounce shot of hard liquor. That means drinking a six-pack of beer is the same as having six shots or six mixed drinks. “Doubles” obviously double the amount of alcohol you are consuming. Expensive drinks are just as damaging as cheap ones.
What We Have Learned About Alcohol and HCV
Several studies have shown that a frighteningly high number of people suffering from alcoholism also have hepatitis C. The numbers range from 11% to 36%. Compare this to the 1.8% HCV infection rate in the general population.4,5 Among alcoholics with liver disease, as many as 51% are infected with HCV. This is 4 to 10 times more frequent than in alcoholics without liver disease.6-11
Studies have shown that alcohol abuse (4 to 5 drinks per day) accelerates the progression of liver damage and fibrosis associated with chronic HCV.1,6,12-21 In a study of 6,664 people in France, excessive alcohol intake doubled the risk of developing cirrhosis and increased the rate of fibrosis progression by 34% per year.22
Research has clearly shown that the severity of liver disease in alcoholics increases in the presence of HCV. In a study from Italy, the incidence of cirrhosis was ten times higher in alcoholics who had HCV than in alcoholics who did not.23 Another study found the survival rate for alcoholics who had HCV antibodies was lower than for alcoholics who did not have HCV infection.24 In addition, several studies have found a significantly increased risk of developing liver cancer among heavy alcohol drinkers who also have HCV.25-28
Alcoholics have an increase in the number and complexity of HCV quasispecies.29 This may explain why alcoholics tend to have a lower response rate to HCV antiviral therapy than nonalcoholics.
Other effects of alcohol may contribute to the greater severity of HCV disease in those who consume it. Some of these effects are listed below.
- possible changes in gene expression
- reduction in the immune system’s ability to respond to and fight off viruses
- inhibition of the liver’s ability to regenerate and repair itself
- stimulation of fibrosis development in the liver
- increased iron deposition in the liver
Most of the studies discussed above clearly show increased liver damage suffered by people with HCV who have more than 4 to 5 drinks of alcohol per day.20,35-37 Other studies show liver damage with as little as one drink per day. Currently, the amount of alcohol consumption that is considered safe for healthy individuals is one drink per day for women and two for men. However, no amount of alcohol can be considered safe if you are infected with HCV. 20,38 People with HCV are strongly urged to eliminate all alcohol consumption.
How Alcohol Damages The Liver
Alcohol is a poisonous chemical that the liver has to break down. As the liver breaks down alcohol, byproducts such as acetaldehyde are formed. Some byproducts produced by the breakdown of alcohol are more toxic to the body than alcohol itself.39
Inflammation is the body’s response to tissue damage or infection. Long-term alcohol use abnormally prolongs the inflammatory process. This leads to an overproduction of free radicals, molecules that can destroy healthy liver tissue and interfere with some of its important functions such as energy production. Alcohol can also interfere with the production of antioxidants. Antioxidants are one of the body’s natural defenses against free radical damage. This combination of alcohol effects can lead to liver damage.40
Cytokines are produced by liver cells and the immune system in response to infection or cell damage. Alcohol use increases cytokine levels.41 Cirrhosis development involves the interaction of certain cytokines and specialized liver cells such as stellate cells. In a normal liver, stellate cells function as storage depots for vitamin A. When activated by cytokines, stellate cells divide rapidly to increase in number. Activated stellate cells lose their vitamin A stores and begin to produce scar tissue. They also constrict blood vessels, reducing the delivery of oxygen to liver cells.42,43 Acetaldehyde, a byproduct of alcohol break down, may activate stellate cells, directly causing liver scarring without inflammation.44-45
Normal scar formation is part of the wound healing process. Cell death and inflammation caused by alcohol can result in abnormal liver scarring. Scarring may distort the liver’s internal structure and interfere with liver function. Scarring in the liver is called fibrosis. Fibrosis that progresses to the point of distorting the structure of the liver is called cirrhosis.
Women, Alcohol, and Hepatitis C
Studies show that women are more susceptible to the damaging effects of alcohol than men are. More alcoholic women die from cirrhosis than alcoholic men.46 The reason for this difference between men and women is not entirely clear.
However, there appears to be several contributing factors.
- Men generally have greater body mass and fluid content than women do. This means women have higher concentrations of alcohol in their blood than men do have after consuming the same amount of alcohol.41,47-51
- Women’s livers appear to metabolize alcohol at a faster rate than men’s do, most likely because women’s livers are larger compared to their body size than those of men.52,53
- Estrogens (female hormones) may add to the effects of alcohol in women’s livers.54
About Alcohol Use
For most people, drinking alcohol is an occasional social activity. For others, drinking alcohol becomes a chronic, progressive disorder called alcoholism. The hallmark of alcoholism is a strong need to drink despite negative consequences including serious health or social problems. Like many diseases, alcoholism has a predictable course and recognizable symptoms. The occurrence of alcoholism is influenced by genetic and environmental factors. We continue to learn more about these factors everyday.
We do not yet have a cure for alcoholism. However, alcoholism is a treatable disorder. Alcoholism is a lifelong problem. Even an alcoholic who has been sober for many years may still be at risk of relapsing and should avoid all alcoholic beverages.
Alcoholism has little to do with what kind of alcohol you drink, how long you have been drinking, or even how much alcohol you drink. The defining characteristic of alcoholism is the uncontrollable need for alcohol. This description helps us understand why most alcoholics cannot just “use a little willpower” to stop drinking. He or she is usually in the grip of a powerful craving for alcohol. This craving can feel as strong as the need for food or water. While some people are able to recover on their own, the majority of alcoholics need outside help. With support and treatment, many people with alcoholism are able to stop drinking and rebuild their lives. Cutting down on drinking does not work for an alcoholic. Stopping alcohol use completely is necessary for successful recovery. This is especially important for people living with chronic hepatitis C.
Even individuals who are determined to stay sober may suffer one or more slips or relapses before achieving long-term sobriety. Relapses are very common and do not signify failure. Nor do they mean a person cannot eventually recover from alcoholism. Every day a recovering alcoholic stays sober prior to a relapse is extremely valuable time. This time is important for both the individual and his or her family. Sober time also gives the liver an opportunity to repair itself. If a relapse occurs, it is very important to try to stop drinking again and to get whatever additional support is needed to abstain from drinking.
Help for Alcohol Abuse
Acknowledging you need help for an alcohol problem is difficult. Many alcoholics do not begin to deal with their alcoholism until a significant life-changing or life-threatening event occurs. Recovering alcoholics often refer to this as “hitting bottom.” The event that represents hitting bottom is different for each person. It depends on your personality and life circumstances. While it is not necessary to hit bottom in order to begin the recovery process, it is often the case. This is because denial is very prevalent in alcoholism. Denial is a coping strategy whereby people avoid dealing with difficult situations by denying that they exist. It is difficult for a person in denial to recognize and understand the effects alcohol has on him or her. This is also true for family members and friends who are frequently in denial with regard to a loved one’s alcoholism.
Many people find the following quiz on drinking helpful. It may help you recognize whether alcohol is a problem in your life.
Do you drink alone when you feel angry or sad?
Does your drinking ever make you late for work?
Does your drinking worry your family?
Do you ever drink after telling yourself you won’t?
Do you ever forget what you did while you were drinking?
Do you get headaches or have a hangover after you have been drinking?
If you answered yes to one or more of these questions, you may have a problem with alcohol.
Many people feel uncomfortable discussing their drinking habits even with a healthcare provider or a personal or spiritual advisor. This often stems from some common misconceptions in our society about alcoholism. There is a myth in our society that an alcohol problem is a sign of moral weakness. As a result, you may feel that to seek help is to admit a shameful defect in your character. Unfortunately, family and friends may support your denial for the same reason. The truth is that alcoholism is a disease. It is no more a sign of weakness than is asthma or diabetes.
Moving Forward
Even if alcohol is taking a significant negative toll on your life, it can be very difficult to begin taking steps to address the problem. This is because what lies ahead is unknown. However, eliminating alcohol from your life has an enormous payoff. It is a chance for a healthier, more rewarding life.
Because alcohol has a tremendous impact on the health of people with chronic hepatitis C, your healthcare provider will probably ask you several questions about your alcohol use. If your healthcare provider determines that you are not alcohol dependent but are involved in a pattern of alcohol abuse, he or she can assist you in the following ways.
- Help you examine the benefits of stopping an unhealthy drinking pattern.
- Help you set a drinking goal for yourself. Some people choose to abstain from alcohol. Others prefer to limit the amount they drink.
- Help you examine situations that trigger unhealthy drinking patterns and develop new ways of handling those situations so you can achieve your drinking goal.
- Recommend a specialist and/or treatment program if you are having difficulty eliminating alcohol from your life.
Your healthcare provider may determine you are dependent on alcohol. He or she may recommend that you see a specialist in diagnosing and treating alcoholism. As hard as this may be to hear, try to understand that your healthcare provider is doing his/her best to help you be well. Ask your provider to explain your treatment choices.
The nature of treatment for alcohol abuse depends on the severity of the problem. It also depends on the resources available in the community. Treatment may include detoxification. Detoxification is the process of safely getting alcohol out of your system. Treatment for alcoholism may involve one or more of the following components: prescription medications, individual counseling, and group counseling. Promising counseling techniques teach recovering alcoholics to identify situations and feelings that trigger the urge to drink. This can help you find new ways to cope with stressful situations that do not include alcohol use. Treatment for alcoholism may be provided in a hospital, residential treatment setting, or on an outpatient basis.
Involvement of friends and family members is important to the recovery process. Many programs offer brief marital counseling and family therapy as part of the treatment process. Some programs also link individuals with vital community resources such as legal assistance, job training, childcare, and parenting classes.
Treatment for alcoholism may require a combination of social support and drug therapy. When faced with the anxiety and fears associated with hepatitis C, you may feel the urge to turn to alcohol. Remember, you are not alone. Reach out and get help to remain alcohol-free.
A few of the common treatment options available for eliminating alcohol from your life are outlined below. Research has shown that no single treatment option is superior to another. Data from a large clinical trial that examined the efficacy of different treatment approaches for alcoholism found that the quality of care is more important than the structure of the treatment delivery.55
Brief Interventions
Many people with alcohol-related problems receive counseling from primary care doctors or nurses in a few office visits.56 This form of treatment is known as brief intervention. It generally consists of straightforward information about the negative consequences of alcohol consumption.
It also gives practical advice on strategies for eliminating alcohol from your life. Information is provided about community resources to achieve alcohol moderation or abstinence.57,58 Most brief interventions are designed to help people at risk for developing alcohol-related problems. They are also used to help people without alcoholism reduce alcohol consumption.
Alcohol-dependent people are encouraged to enter specialized treatment programs where the goal is complete abstinence.57
Structured Outpatient Therapy
Structured outpatient treatment for alcohol abuse usually spans several months. It typically involves educational lectures, group therapy, and one-on-one counseling. The objectives and activities of outpatient treatment typically include a combination of the following:
- develop an understanding of substance abuse and addiction
- identify how alcohol has affected the participant’s life
- instill greater self-awareness
- identify and understand factors that contribute to alcohol abuse
- learn effective communication skills
- understand factors that contribute to relapse and how to prevent them
- begin participation in a community-based support program such as Alcoholics Anonymous (AA)
Inpatient Therapy
Residential or inpatient treatment takes place in a dormitory-like setting. Clients often share a room and live in the facility for at least 30 days. Some clients stay for several months depending on individual circumstances and needs. Programs vary from one facility to another, but many are based on 12-step program principles such as those of AA. The social setting allows people who are facing a similar challenge to share experiences and support one another. Typically, clients attend lectures, meetings, group therapy, and individual therapy throughout the day.
In a residential facility, a client’s physical and mental status can be closely monitored. The temporary protection of a residential treatment facility provides clients a safe place to begin rebuilding their lives without the distractions of work or other pressures. An essential component of residential treatment is making plans for how to maintain sobriety after leaving the facility.
Some facilities offer part-time residential treatment for clients who cannot or do not choose to take time off work. Clients continue to attend work, but spend the rest of their time in the treatment facility. These programs typically last 30 to 60 days.
Sober-living homes are another residential treatment option. Clients who have been through full-time residential treatment may transition to a sober-living home after completing their primary program. Clients live in the facility for an extended period while working on rebuilding their lives. This type of facility is often useful for people who have been through treatment in the past, but have relapsed after returning to their usual environment.
Couples Therapy
Evidence indicates that involvement of a nonalcoholic partner in a treatment program can improve participation by the person with alcoholism. This support increases the likelihood that the alcoholic person will change his or her drinking behavior after treatment ends.59 There are different approaches to couples therapy. Most of these include shared activities, and learning communication and conflict resolution skills.60 Partners of people in treatment for alcohol abuse or dependence are often encouraged to also discontinue drinking alcohol. It can be quite difficult for an alcoholic to abstain if his or her partner continues to drink.
Motivational Enhancement Therapy
Motivational enhancement therapy (MET) was developed in the late 1990’s for a large clinical trial called Project MATCH sponsored by the National Institute on Alcohol Abuse and Alcoholism. MET continues to be used as a successful treatment approach for alcoholism. It begins with the assumption that the responsibility and capacity for change lie within the individual.61,62 Therapy begins by providing individualized feedback about the effects of the person’s drinking. The therapist and client explore the benefits of abstinence. Together, they review treatment options and design a plan to implement treatment goals.
Pharmacotherapy
Medications are available for blocking alcohol-brain interactions that might promote alcoholism. People with HCV should not take any of these medications before speaking to a healthcare provider because taking one of these medications may be harmful to the liver. Your healthcare provider will review the drugs available and determine if any are appropriate for you.
Self-help Programs
Self-help groups are the most commonly used programs for alcohol-related problems.163 Alcoholics Anonymous is the most widely known of these self-help groups. AA describes itself as a “worldwide fellowship of men and women who help each other to stay sober.” It offers a 12-step program that has been effective for many people seeking to eliminate alcohol from their lives. Alcoholics can become involved with AA before entering professional treatment for alcoholism, as a part of it, or as aftercare. The AA approach is well known, but the program has not been studied in clinical trials.64 This is due to an essential requirement of the program that people remain anonymous. In AA, only first names are used.
The benefits of AA may be partially due to the replacement of the participant’s social network of drinking friends with a fellowship of AA members who can provide motivation and support for maintaining abstinence.63,65 AA’s approach often results in the development of new coping skills. Many of these skills are similar to those taught in more structured treatment settings. These skills can lead to reduced alcohol consumption.63,66
Most treatment programs for alcoholism include AA meetings. AA is generally recognized as an effective support program for recovering alcoholics. However, not everyone responds to AA’s style and message. If AA is not for you, other recovery programs are available. Even those who are helped by AA find it usually works best in combination with other forms of treatment. This may include individual counseling and/or medical care.
The Final Word
No studies have ever determined a safe amount of alcohol to drink. If you have HCV, the authors of this book strongly recommend you eliminate all alcohol from your life. you will live better and longer!
note: Much of the information in this chapter was obtained from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). For additional information, visit the NIAAA Internet site at www.niaaa.nih.gov.
How to Cut Down on Your Drinking
How to Cut Down on Your Drinking
NATIONAL INSTITUTE ON ALCOHOL ABUSE AND ALCOHOLISM
NATIONAL INSTITUTES OF HEALTH
How to Cut Down on Your Drinking
If you are drinking too much, you can improve your life and health by cutting down. How do you know if you drink too much? Read these questions and answer “yes” or “no”:
- Do you drink alone when you feel angry or sad?
- Does your drinking ever make you late for work?
- Does your drinking worry your family?
- Do you ever drink after telling yourself you won’t?
- Do you ever forget what you did while you were drinking?
- Do you get headaches or have a hang-over after you have been drinking?
If you answered “yes” to any of these questions, you may have a drinking problem. Check with your doctor to be sure. Your doctor will be able to tell you whether you should cut down or abstain. If you are alcoholic or have other medical problems, you should not just cut down on your drinking–you should stop drinking completely. Your doctor will advise you about what is right for you.
If your doctor tells you to cut down on your drinking, these steps can help you:
1. Write your reasons for cutting down or stopping.
Why do you want to drink less? There are many reasons why you may want to cut down or stop drinking. You may want to improve your health, sleep better, or get along better with your family or friends. Make a list of the reasons you want to drink less.
2. Set a drinking goal.
Choose a limit for how much you will drink. You may choose to cut down or not to drink at all. If you are cutting down, keep below these limits:
Women: No more than one drink a day
Men: No more than two drinks a day
A drink is:
- a 12-ounce bottle of beer;
- a 5-ounce glass of wine; or
- a 1 1/2-ounce shot of liquor.
These limits may be too high for some people who have certain medical problems or who are older. Talk with your doctor about the limit that is right for you.
Now–write your drinking goal on a piece of paper. Put it where you can see it, such as on your refrigerator or bathroom mirror. Your paper might look like this:
My drinking goal
• I will start on this day ____________.
• I will not drink more than ______ drinks in 1 day.
• I will not drink more than ______ drinks in 1 week.
or
• I will stop drinking alcohol.
3. Keep a “diary” of your drinking.
To help you reach your goal, keep a “diary” of your drinking. For example, write down every time you have a drink for 1 week. Try to keep your diary for 3 or 4 weeks. This will show you how much you drink and when. You may be surprised. How different is your goal from the amount you drink now? Use the “drinking diary” below to write down when you drink.
| Week: | |||
| # of drinks | type of drinks | place consumed | |
| Mon. | |||
| Tues. | |||
| Wed. | |||
| Thurs. | |||
| Fri. | |||
| Sat. | |||
| Sun. | |||
| Week: | |||
| # of drinks | type of drinks | place consumed | |
| Mon. | |||
| Tues. | |||
| Wed. | |||
| Thurs. | |||
| Fri. | |||
| Sat. | |||
| Sun. | |||
| Week: | |||
| # of drinks | type of drinks | place consumed | |
| Mon. | |||
| Tues. | |||
| Wed. | |||
| Thurs. | |||
| Fri. | |||
| Sat. | |||
| Sun. | |||
| Week: | |||
| # of drinks | type of drinks | place consumed | |
| Mon. | |||
| Tues. | |||
| Wed. | |||
| Thurs. | |||
| Fri. | |||
| Sat. | |||
| Sun. | |||
Now you know why you want to drink less and you have a goal. There are many ways you can help yourself to cut down. Try these tips:
Watch it at home.
Keep a small amount or no alcohol at home. Don’t keep temptations around.
Drink slowly.
When you drink, sip your drink slowly. Take a break of 1 hour between drinks. Drink soda, water, or juice after a drink with alcohol. Do not drink on an empty stomach! Eat food when you are drinking.
Take a break from alcohol.
Pick a day or two each week when you will not drink at all. Then, try to stop drinking for 1 week. Think about how you feel physically and emotionally on these days. When you succeed and feel better, you may find it easier to cut down for good.
Learn how to say NO.
You do not have to drink when other people drink. You do not have to take a drink that is given to you. Practice ways to say no politely. For example, you can tell people you feel better when you drink less. Stay away from people who give you a hard time about not drinking.
Stay active.
What would you like to do instead of drinking? Use the time and money spent on drinking to do something fun with your family or friends. Go out to eat, see a movie, or play sports or a game.
Get support.
Cutting down on your drinking may be difficult at times. Ask your family and friends for support to help you reach your goal. Talk to your doctor if you are having trouble cutting down. Get the help you need to reach your goal.
Watch out for temptations.
Watch out for people, places, or times that make you drink, even if you do not want to. Stay away from people who drink a lot or bars where you used to go. Plan ahead of time what you will do to avoid drinking when you are tempted.
Do not drink when you are angry or upset or have a bad day. These are habits you need to break if you want to drink less.
DO NOT GIVE UP!
Most people do not cut down or give up drinking all at once. Just like a diet, it is not easy to change. That is okay. If you do not reach your goal the first time, try again.
Remember, get support from people who care about you and want to help. Do not give up!
All material in this pamphlet is free of copyright restrictions and may be reproduced or duplicated without permission from the Institute; citation of the source is appreciated.
NIH Pub No. 96-3770
Printed 1996
Updated: May 28, 2001
Resources
For more information on alcohol abuse and alcoholism, contact the following organizations.
Al-Anon Family group Headquarters
1600 Corporate Landing Parkway
Virginia Beach, VA 23454-5617
Internet address: www.al-anon.alateen.org
Al-Anon headquarters provides referrals to local Al-Anon groups, which are support groups for spouses and other significant adults in an alcoholic person’s life. They also provide referrals to Alateen groups, which offer support to children of alcoholics. Locations of Al-Anon or Alateen meetings worldwide can be obtained by calling the toll-free number, (888) 425-2666, Monday through Friday, 8 AM to 6 PM (EST). Informational materials can be obtained on line or by calling (757) 563-1600
Alcoholics Anonymous (AA) World services
Box 459
New York, NY 10163
(212) 870-3400
Internet address: www.alcoholics-anonymous.org
This organization makes referrals to local AA groups and provides informational materials about the AA program. Many cities and towns also have a local AA office listed in the telephone directory.
Faces and Recovery
1010 Vermont Ave. #708
Washington, DC 20005
(202) 737-0690
Internet address: www.facesandvoicesofrecovery.org
Faces & Voices of Recovery is a national campaign of individuals and organizations joining together with a united voice to advocate for public action to deliver the power, possibility and proof of recovery. Faces & Voices of Recovery is governed by a diverse group of recovery advocates from around the country and supports local recovery advocacy by increasing access to research, policy, organizing and technical support; facilitating relationships among local and regional groups; improving access to policymakers and the media; and providing a national rallying point for recovery advocates.
National Council for Behavorial Health
1400 K Street NW, Suite 400
Washington, DC 20005
(202) 684-7457
Internet address: thenationalcouncil.org
The National Council for Behavioral Health is the unifying voice of America’s health care organizations that deliver mental health and addictions treatment and services. Together with our 3,381 member organizations serving over 10 million adults, children and families living with mental illnesses and addictions.
National Institute on Alcohol Abuse and Alcoholism (nIAAA)
5635 Fishers Lane, MSC 9304
Bethesda, MD 20892-9304
(301) 443-3860
Internet address: www.niaaa.nih.gov
NIAAA is part of the National Institutes of Health. NIAAA’s mission is to provide leadership in the national effort to reduce alcohol-related problems. The NIAAA Internet site has an abundance of information about alcohol-related problems in both Spanish and English.
Substance Abuse Treatment Facility Locator
(800) 662–4357
Internet address: https://www.samhsa.gov/find-treatment
Offers alcohol and drug information and treatment referral assistance. (This service is provided by the Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services.)
References
Information in this section has been updated and adapted from Hepatitis C Choices 4th Edition, Alcohol and Hepatitis C written by Douglas R. LaBrecque, MD and Lorren Sandt
- Wiley TE, McCarthy M, Breidi L, McCarthy M, Layden TJ. Impact of alcohol on the histological and clinical progression of hepatitis C infection. Hepatology. 1998;28(3):805-809.
- Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. Lancet. 997;349(9055):825832.
- Zeuzem S. Heterogeneous virologic response rates to interferon-based therapy in patients with chronic hepatitis C: who responds less well? Ann Intern Med. 2004;140(5):370-81.
- Regev A, Jeffers LJ. Hepatitis C and alcohol. Alcohol Clin Exp Res. 1999;23(9):1543-1551.
- Schiff ER. The alcoholic patient with hepatitis C virus infection. Am J Med. 1999;107(6B):95-99S.
- Ohta S, Watanabe Y, Nakajima T. Consumption of alcohol in the presence of hepatitis C virus is an additive risk for liver damage. Prev Med. 1998;27(3):461-469.
- Caldwell SH, Jeffers LJ, Ditomaso A, et al. Antibody to hepatitis C is common among patients with alcoholic liver disease with and without risk factors. Am J Gastroenterol. 1991;86(9):1219-1223.
- Pares A, Barrera JM, Caballeria J, et al. Hepatitis C virus antibodies in chronic alcoholic patients: association with severity of liver injury. Hepatology. 1990;12(6):1295-1299.
- Coelho-Little ME, Jeffers LJ, Bernstein DE, et al. Hepatitis C virus in alcoholic patients with and without clinically apparent liver disease. Alcohol Clin Exp Res. 1995;19(5):1173-1176.
- Mendenhall CL, Seeff L, Diehl AM, et al. Antibodies to hepatitis B virus and hepatitis C virus in alcoholic hepatitis and cirrhosis: their prevalence and clinical relevance. Hepatology. 1991;14(4 Pt 1):581-589.
- Mendenhall CL, Moritz T, Rouster S, et al. Epidemiology of hepatitis C among veterans with alcoholic liver disease. Am J Gastroenterol. 1993;88(7):1022-1026.
- Corrao G, Arico S. Independent and combined action of hepatitis C virus infection and alcohol consumption on the risk of symptomatic liver cirrhosis. Hepatology. 1998;27(4):914-919.
- Pessione F, Degos F, Marcellin P, et al. Effect of alcohol consumption on serum hepatitis C virus RNA and histological lesions in chronic hepatitis C. Hepatology. 1998;27(6):1717-1722.
- Ostapowicz G, Watson KJ, Locarnini SA, Desmond PV. Role of alcohol in the progression of liver disease caused by hepatitis C virus infection. Hepatology. 1998;27(6):1730-1735.
- Khan MH, Thomas L, Byth K, et al. How much does alcohol contribute to the variability of hepatic fibrosis in chronic hepatitis C? J Gastroenterol Hepatol. 1998;13(4):419-426.
- Kondili LA, Tosti ME, Szklo M, et al. The relationships of chronic hepatitis and cirrhosis to alcohol intake, hepatitis B and C, and delta virus infection: a case-control study in Albania. Epidemiol Infect. 1998;121(2):391-395.
- Frieden TR, Ozick L, McCord C, et al. Chronic liver disease in central Harlem: the role of alcohol and viral hepatitis. Hepatology. 1999;29(3):883-888.
- Nevins CL, Malaty H, Velez ME, Anand BS. Interaction of alcohol and hepatitis C virus infection on severity of liver disease. Dig Dis Sci. 1999;44(6):1236-1242.
- Loguercio C, Di Pierro M, Di Marino MP, et al. Drinking habits of subjects with hepatitis C virus-related chronic liver disease: prevalence and effect on clinical, virological and pathological aspects. Alcohol Alcohol. 2000;35(3):296-301.
- Monto A, Patel K, Bostrom A, et al. Risks of a range of alcohol intake on hepatitis C-related fibrosis. Hepatology. 2004;39(3):826-34.
- Bellentani S, Saccoccio G, Costa G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. Gut. 1997;41(6):845-50.
- Roudot-Thoraval F, Bastie A, Pawlotsky JM, Dhumeaux D. Epidemiological factors affecting the severity of hepatitis C virus-related liver disease: a French survey of 6,664 patients. Hepatology. 1997;26(2):485-490.
- Bellentani S, Tiribelli C, Saccoccio G, et al. Prevalence of chronic liver disease in the general population of northern Italy: the Dionysos Study. Hepatology. 1994;20(6):1442-1449.
- Takase S, Tsutsumi M, Kawahara H, et al. The alcohol-altered liver membrane antibody and hepatitis C virus infection in the progression of alcoholic liver disease. Hepatology. 1993;17(1):9-13.
- Donato F, Tagger A, Chiesa R, et al. Hepatitis B and C virus infection, alcohol drinking, and hepatocellular carcinoma: a case-control study in Italy. Brescia HCC Study. Hepatology. 1997;26(3):579-584.
- Mori M, Hara M, Wada I, et al. Prospective study of hepatitis B and C viral infections, cigarette smoking, alcohol consumption, and other factors associated with hepatocellular carcinoma risk in Japan. Am J Epidemiol. 2000;151(2):131-139.
- Khan KN, Yatsuhashi H. Effect of alcohol consumption on the progression of hepatitis C virus infection and risk of hepatocellular carcinoma in Japanese patients. Alcohol Alcohol. 2000;35(3):286-295.
- Noda K, Yoshihara H, Suzuki K, et al. Progression of type C chronic hepatitis to liver cirrhosis and hepatocellular carcinoma -its relationship to alcohol drinking and the age of transfusion. Alcohol Clin Exp Res. 1996;20(1 Suppl):95-100A.
- Sherman KE, Rouster SD, Mendenhall C, Thee D. Hepatitis C RNA quasispecies complexity in patients with alcoholic liver disease. Hepatology. 1999;30(1):265-270.
- Ohnishi K, Matsuo S, Matsutani K, et al. Interferon therapy for chronic hepatitis C in habitual drinkers: comparison with chronic hepatitis C in infrequent drinkers. Am J Gastroenterol. 1996;91(7):1374-1379.
- Okazaki T, Yoshihara H, Suzuki K, et al. Efficacy of interferon therapy in patients with chronic hepatitis C. Comparison between non-drinkers and drinkers. Scand J Gastroenterol. 1994;29(11):1039-1043.
- Tabone M, Sidoli L, Laudi C, et al. Alcohol abstinence does not offset the strong negative effect of lifetime alcohol consumption on the outcome of interferon therapy. J Viral Hepat. 2002;9(4):288-94.
- Loguercio C, Di Pierro M, Di Marino MP, et al. Drinking habits of subjects with hepatitis C virus-related chronic liver disease: prevalence and effect on clinical, virological and pathological aspects. Alcohol Alcohol. 2000;35(3):296-301.
- National Institutes of Health Consensus Development Conference Statement: Management of hepatitis C 2002 (June 10-12, 2002). Gastroenterology. 2002;123(6):2082-99.
- Hezode C, Lonjon I, Roudot-Thoraval F, Pawlotsky JM, Zafrani ES, Dhumeaux D. Impact of moderate alcohol consumption on histological activity and fibrosis in patients with chronic hepatitis C, and specific influence of steatosis: a prospective study. Aliment Pharmacol Ther. 2003;17(8):1031-7.
- Hutchinson SJ, Bird SM, Goldherg DJ. Influence of alcohol on the progression of hepatitis C virus infection: a meta-analysis. Clin Gastroenterol Hepatol. 2005 Nov;3(11):1150-9.
- Delarocque-Astagneau E, et al. Past excessive alcohol consumption: a major determinant of severe liver disease among newly referred hepatitis C virus infected patients in hepatiology reference centers, France 2001. Ann Epidemiol. 2005 Se:15(8):551-7
- Westin J, Lagging LM, Spak F, et al. Moderate alcohol intake increases fibrosis progression in untreated patients with hepatitis C virus infection. J Viral Hepat. 2002;9(3):235-41.
- Ma X, Svegliati-Baroni G, Poniachik J, et al. Collagen synthesis by liver stellate cells is released from its normal feedback regulation by acetaldehyde-induced modification of the carboxyl-terminal propeptide of procollagen. Alcohol Clin Exp Res. 1997;21(7):1204-1211.
- McClain C, Shedlofsky S, Barve S, Hill D. Cytokines and alcoholic liver disease. Alcohol Health Res World. 1997;21(4):317-320.
- Lands WE. Cellular signals in alcohol-induced liver injury: a review. Alcohol Clin Exp Res. 1995;19(4):928-938.
- Maher J, Friedman S. Pathogenesis of hepatic fibrosis. In: Hall P (Ed.). Alcoholic Liver Disease: Pathology and Pathogenesis. London, England. Oxford University Press. 1995.
- Lieber CS. Hepatic and other medical disorders of alcoholism: from pathogenesis to treatment. J Stud Alcohol. 1998;59(1):9-25.
- Lieber CS. Alcoholic liver disease: new insights in pathogenesis lead to new treatments. J Hepatol. 2000;32(1 Suppl):113-128.
- 45.Kurose I, Higuchi H, Kato S, Miura S, Ishii H. Ethanol-induced oxidative stress in the liver. Alcohol Clin Exp Res. 1996;20(1 Suppl):77-85A.
- Gavaler J, Arria A. Increases susceptibility of women to alcoholic liver disease: Artifactual or real? In: Hall P (Ed.). Alcoholic Liver Disease: Pathology and Pathogenesis. London, England. Oxford University Press. 1995.
- Tuyns AJ, Pequignot G. Greater risk of ascitic cirrhosis in females in relation to alcohol consumption. Int J Epidemiol. 1984;13(1):53-57.
- Nicholls P, Edwards G, Kyle E. Alcoholics admitted to four hospitals in England. II. General and cause-specific mortality. Q J Stud Alcohol. 1974;35(3):841-855.
- 49.Patwardhan RV, Desmond PV, Johnson RF, Schenker S. Impaired elimination of caffeine by oral contraceptive steroids. J Lab Clin Med. 1980;95(4):603-608.
- Johnson RD, Williams R. Genetic and environmental factors in the individual susceptibility to the development of alcoholic liver disease. Alcohol Alcohol. 1985;20(2):137-160.
- Frezza M, di Padova C, Pozzato G, et al. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322(2):95-99.
- Taylor JL, Dolhert N, Friedman L, et al. Alcohol elimination and simulator performance of male and female aviators: a preliminary report. Aviat Space Environ Med. 1996;67(5):407-413.
- Kwo PY, Ramchandani VA, O’Connor S, et al. Gender differences in alcohol metabolism: relationship to liver volume and effect of adjusting for body mass. Gastroenterology. 1998;115(6):1552-1557.
- Li T, Beard J, Orr W, et al. Gender and ethnic differences in alcohol metabolism. Alcohol Clin Exp Res. 1998;22(3):771-772.
- Anon. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):7-29.
- Fleming M, Manwell LB. Brief intervention in primary care settings. A primary treatment method for at-risk, problem, and dependent drinkers. Alcohol Res Health. 1999;23(2):128-137.
- Alcohol Alert No. 43. Brief intervention for alcohol problems. National Institute on Alcohol Abuse and Alcoholism. Bethesda, Maryland. 1999.
- DiClemente CC, Bellino LE, Neavins TM. Motivation for change and alcoholism treatment. Alcohol Res Health. 1999;23(2):86-92.
- Steinglass P. Family Therapy: Alcohol. In: Galanter M, Kleber H, (Eds.). The American Psychiatric Press Textbook of Substance Abuse Treatment. American Psychiatric Press. Washington, DC. 1999.
- 60.O’Farrell TJ. Marital and family therapy in alcoholism treatment. J Subst Abuse Treat. 1989;6(1):23-29.
- Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):729.
- Miller WR, Zweben A, DiClemente CC, Rychatrik R. Motivational Enhancement Therapy Manual. NIH Pub. No. 94-3723. National Institutes of Health. Rockville, Maryland. 1995.
- Humphreys K, Mankowski ES, Moos RH, Finney JW. Do enhanced friendship networks and active coping mediate the effect of self-help groups on substance abuse? Ann Behav Med. 1999;21(1):54-60.
- Tonigan JS, Toscova R, Miller WR. Meta-analysis of the literature on Alcoholics Anonymous: sample and study characteristics moderate findings. J Stud Alcohol. 1996;57(1):65-72.
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93(9):1313-1333.
- Morgenstern J, Labouvie E, McCrady BS, et al. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. J Consult Clin Psychol. 1997;65(5):768-777.
